Tuesday, November 22, 2016
Wednesday, November 9, 2016
MEET WITH US IN SAN DIEGO AT SOCIETY FOR NEUROSCIENCE!
The emka & SCIREQ team will be attending the Society for Neuroscience 2016 conference in San Diego! We will present and demonstrate our wide range of preclinical instruments for neuro, pulmonary and cardio studies. Come by booth #3533 and speak with our experienced team about our solutions for physiology, pharmacology and toxicology research.
A special focus on optogenetics
Optogenetic studies targeting respiratory centers in the brain stem can be paired with whole body plethysmography (WBP) to measure pulmonary function.
 » Our WBP chambers pair with fibre optic cables to offer real-time assessment of lung function changes resulting from optical manipulation.
» Our WBP chambers pair with fibre optic cables to offer real-time assessment of lung function changes resulting from optical manipulation.
» Does not require anaesthetics, which can depress the neural-network controlling respiration.
» Conscious, freely moving subjects that have the ability to respond to real-time optical challenges.
» Swivel/tether system for measurement of other physiological parameters (ECG, EEG) or blood sampling following injections.
» Easily integrated with gas challenges (CO2/O2) to further induce or inhibit signaling pathways.
» Measures ventilatory parameters: Respiratory Rate (RR), estimated Tidal Volume (VT), Minute Ventilation (V) or Periodic breathing
Telemetry
easyTEL implantable system transmits physiological data from conscious freely moving laboratory animals. Our range of implants offers the ability to record the following parameters, depending on your study needs:
» Biopotential (ECG, EEG, EMG)
» Blood pressure
» Temperature
» Activity from acceleration
Click here to schedule a meeting with one of our specialists during SFN 2016.
A special focus on optogenetics
Optogenetic studies targeting respiratory centers in the brain stem can be paired with whole body plethysmography (WBP) to measure pulmonary function.
 » Our WBP chambers pair with fibre optic cables to offer real-time assessment of lung function changes resulting from optical manipulation.
» Our WBP chambers pair with fibre optic cables to offer real-time assessment of lung function changes resulting from optical manipulation.» Does not require anaesthetics, which can depress the neural-network controlling respiration.
» Conscious, freely moving subjects that have the ability to respond to real-time optical challenges.
» Swivel/tether system for measurement of other physiological parameters (ECG, EEG) or blood sampling following injections.
» Easily integrated with gas challenges (CO2/O2) to further induce or inhibit signaling pathways.
» Measures ventilatory parameters: Respiratory Rate (RR), estimated Tidal Volume (VT), Minute Ventilation (V) or Periodic breathing
Telemetry
easyTEL implantable system transmits physiological data from conscious freely moving laboratory animals. Our range of implants offers the ability to record the following parameters, depending on your study needs:
» Biopotential (ECG, EEG, EMG)
» Blood pressure
» Temperature
» Activity from acceleration
Click here to schedule a meeting with one of our specialists during SFN 2016.
Friday, November 4, 2016
THANK YOU UNIVERSITY OF WISCONSIN-MADISON!

Thank
you to Drs. Teodorescu and Broytman at the University of Wisconsin-Madison for
hosting an introductory workshop and seminar on Lung Function Measurements in
Rodents. Research and Development Manager, Liah Fereydoonzad, and Application
Specialist, John Morse, worked with participants at the workshop to perform an
automated dose-response study in an allergic model with the flexiVent.
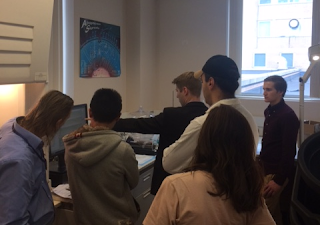
The seminar presentation discussed a variety of solutions for in vivo lung physiology, from non-invasive whole body plethysmography to detailed respiratory mechanics with the flexiVent. An application specific approach to the outcomes of each method was presented, as the detail of outcomes is determined by the invasiveness of the technique1.

Please contact us to find out more about lung function measurements or if you are interested in hosting a similar event! www.scireq.com
1 J. H. Bates and C. G. Irvin,
"Measuring lung function in mice: the phenotyping uncertainty
principle.," Journal of Applied Physiology, vol. 94, p. 1297, 2003.
Subscribe to:
Posts (Atom)


